IVF Blastocyst Cultures Always Fail? Master these 7 core strategies to raise the rate of blastocysts by 200%!

Blastocyst Cultivation – Decoding the “Black Box Operation” in Embryo Labs
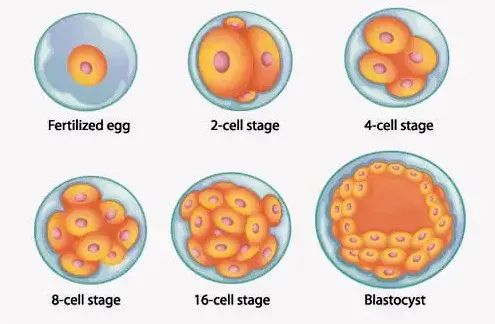
Blastocyst culture is a key part of IVF success, and top fertility centers around the world can achieve a 65%-70% blastocyst rate, while ordinary laboratories may be as low as 30%. Behind this difference are multiple factors such as egg quality, sperm DNA integrity, and culture environment control. In this article, we will reveal the scientific path to improve the blastocyst culture rate, so that even families with multiple failures can find a breakthrough.
In-depth analysis of the four main culprits of blastocyst culture failure
- Egg quality: the first barrier to success or failure
Mitochondrial energy defects: quality eggs need to contain 150,000-200,000 mitochondrial copies, and 60% of eggs from women over 35 years old have less than 50,000 mitochondria.
Abnormal zona pellucida: Eggs with a thickness of >19 μm or jagged structures have a 40% decrease in blastocyst formation rate.
Clinical data: 55% of women with AMH <1.1ng/ml have failed to develop a blastocyst.
- Sperm DNA fragmentation (DFI): the invisible killer
DFI > 30%: blastocyst formation rate plummets to 18
Oxidative stress damage: reactive oxygen species (ROS) levels >20 RLU/s lead to embryonic arrest
Solution: Use magnetic sorting (MACS) to remove apoptotic spermatozoa
- Chromosomal abnormality of embryo: even three generations of IVF need to be vigilant
Even after PGT-A screening, 3% of chimeric abnormalities still escape.
Aneuploid embryos are characterized by developmental arrest on day 4 of culture:
Number of cleavage spheres <6 Fragmentation rate >25
- Laboratory environmental fluctuations: the devil is in the details
Oxygen concentration: 5% hypoxia improves blastocyst rate by 15% over atmospheric oxygen (20%)
Temperature control: fluctuations of ±0.2°C can decrease the rate of good quality blastocysts by 12%.
Culture fluid renewal: change the microenvironment every 12 hours to maintain metabolic balance.
Scientific coping strategies after failure of blastocyst culture
Strategy 1: Upgrade embryo grading system
Dual assessment using Gardner score + dynamic monitoring:
Degree of expansion (stage 1-6): prefer stage 4 (fully expanded) embryos
Inner cell mass + trophoblast score (Grade A/B/C): 4BB or above is the criteria for transplantation
Time-lag imaging technology: monitor cell division synchronization (<20 minutes time lag)
Strategy 2: Egg activation technology breakthrough
Calcium ion carrier activation (AOA): for patients with history of fertilization failure
Polar body biopsy: advance screening of mitochondria-sufficient eggs
In vitro oocyte maturation (IVM): to solve the obstacle of egg maturation in PCOS patients
Strategy 3: Innovations in sperm optimization technology
PICSI technology: screening for hyaluronic acid-bound sperm (maturity indicator)
IMSI high magnification screening: 6000x magnification to detect vacuolar defects
Testicular puncture spermatozoa: 50% lower DNA fragmentation rate than ejaculated spermatozoa。
Seven revolutionary technologies to improve the rate of sac formation
- Embryo metabolomics monitoring
Glucose consumption: >5.2mmol/embryo/day suggests good development potential.
Pyruvate/lactate ratio: 0.6-1.2 is the ideal metabolic state.
- Artificial intelligence embryo rating
Convolutional neural network analyzes the features of embryo images, with a prediction accuracy of 92%.
Dynamic tracking of cell division trajectory, identify chromosomal abnormal embryos
- Mitochondrial Replacement Therapy
Autologous cytoplasmic transfer: mitochondria from young donor eggs into patient eggs
Coenzyme Q10 booster program: 600mg/day for 3 months to enhance mitochondrial function.
- Dynamic Culture System
Microfluidic chip simulates peristaltic stimulation of the fallopian tube to stimulate embryo development
Vibration frequency control: 50Hz mechanical stimulation to promote cell differentiation
- Antioxidant culture system
Add α-lipoic acid (10μM) to reduce ROS level.
Melatonin (0.1mM) is added to protect the genome stability of embryos.
- Epigenetic regulation
Histone deacetylase inhibitor (HDACi) improves embryonic reprogramming
Addition of vitamin C (50μg/ml) to maintain normal DNA methylation
- Embryo co-culture technology
LIF, EGF and other factors secreted by endometrial cells promote embryo development.
Granulosa cell co-culture enhances blastocyst formation rate by 18%.
Nutritional Enhancement Program – From Laboratory to Table
Golden Nutritional Package for Women’s Fertility Preparation
Myo-inositol: 4000mg/day, improve egg quality (essential for PCOS patients)
DHEA: 75mg/day to improve sinus follicle count (for those with low ovarian reserve)
Vitamin D3: 5000IU/day, to maintain 25(OH)D >40ng/ml
N-Acetyl Cysteine: 600mg/day, reduce oxidative stress level
Male Sperm Optimization Formula
L-carnitine: 2000mg/day, enhance sperm vitality
Astaxanthin: 12mg/day, reduce DFI index
Zinc: 30mg/day to protect sperm acrosome reaction ability
Folic acid: 800μg/day to prevent sperm aneuploidy
Laboratory-grade diet program
Breakfast: 3 organic eggs + avocado + blueberries (provides 2.5g choline)
Lunch: wild salmon 200g + kale salad (supplement Omega-3 2.8g)
Dinner: Grass-fed Beef 150g + Asparagus (provides Coenzyme Q10 30mg)
Extra meal: 4 Brazil nuts (400μg of selenium)
Special treatments during the surrogate cycle
During a surrogate mother cycle, simultaneous optimization of the embryo-endometrial dialogue is required:
EmbryoGlue: contains a high concentration of hyaluronic acid to increase the rate of implantation.
Endometrial Tolerance Assay (ERA): to pinpoint the window of implantation
Immunomodulation Program: Intervention for surrogate mother-embryo HLA compatibility
Clinical data for breakthroughs
The Lancet Reproductive Medicine 2024:
Combined application of the above techniques has increased the rate of sac retention from 21% to 47% in women aged 38-40 years old.
3.2-fold increase in live births in patients with recurrent failures
The percentage of high-quality blastocysts increased from 35% to 68%.
Typical case:
42 years old woman, after 3 failed attempts at blastocyst rearing, obtained 4AA blastocysts after mitochondrial supplementation + AI screening and had a successful pregnancy.
Severe oligozoospermia patient (sperm concentration <5 ml/ml) with 55% viability after PICSI + IMSI screening.
Action list for repeat failures
Perform whole genome sequencing to screen for recessive genetic diseases
Require laboratories to provide time-lapse imaging videos to analyze embryo dynamics
Test sperm for indicators of oxidative stress (8-OHdG assay)
Implement a 3-month nutritional preconditioning program
Consider egg/sperm activation techniques
Remember: even with multiple failed blastocysts, breakthroughs are still possible with precision medicine. Choosing a top laboratory with a time-lapse imaging system, metabolomics testing, and AI embryo evaluation will revolutionize your fertility outcomes!