Surrogate Mothers in 2025: A Global Guide to Legal, Medical, and Ethical Challenges

Introduction
In 2025, the demand for surrogate mothers continues to grow globally, driven by advancements in reproductive technology and evolving societal norms. However, this practice remains fraught with legal ambiguities, ethical dilemmas, and health risks—especially for surrogate mothers. This guide explores the critical considerations for intended parents and surrogate mothers, emphasizing compliance with international standards, medical best practices, and ethical safeguards.
Section 1: Legal Preparation for Surrogate Mothers
Surrogate mothers must prioritize legal safeguards to avoid exploitation. Key steps include:
- Agency Accreditation
Choose agencies accredited by the International Association for Assisted Reproduction (IARC). These organizations adhere to strict ethical guidelines and minimize subcontracting risks, ensuring surrogate mothers receive fair compensation and medical care. - Contract Essentials
Contracts must clarify:
- Medical Malpractice Compensation: Surrogate mothers should demand coverage for complications like preterm labor or gestational diabetes.
- Privacy Protections: Strict confidentiality clauses to prevent unauthorized disclosure of personal or medical data.
- Termination Clauses: Clear exit mechanisms for surrogate mothers in cases of health risks or ethical concerns.
- Financial Safeguards
Funds should be held in third-party escrow accounts to ensure timely payments. In 2025, blockchain-based smart contracts are increasingly used in countries like Georgia to automate payments and enhance transparency.
Section 2: Medical Process and Surrogate Mothers’ Health
Surrogate mothers undergo rigorous medical protocols to ensure safety and success:
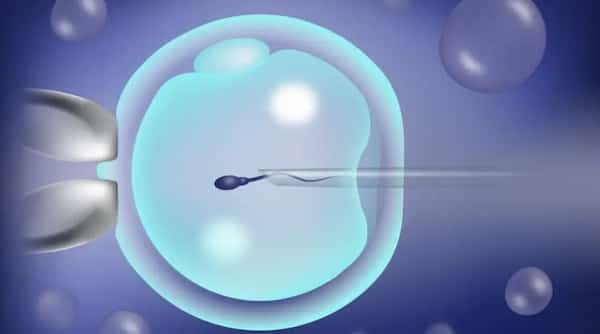
- Embryo Screening (PGT Technology)
Preimplantation genetic testing (PGT) screens embryos for chromosomal abnormalities, boosting transfer success rates to 72%. However, ethical debates persist over non-medical sex selection, which has led to forced abortions in unregulated markets like India. - Cycle Synchronization
Hormonal regimens align the surrogate mother’s cycle with the egg donor’s, requiring precision within 48 hours. Estrogen and progesterone therapies must be monitored to avoid hyperstimulation risks. - Delivery Rights
Contracts should specify the surrogate mother’s right to choose vaginal delivery or cesarean section. Cross-border surrogacy requires pre-planning for the newborn’s citizenship and passport applications.
Section 3: Postnatal Rights and Long-Term Protections for Surrogate Mothers
Post-delivery, surrogate mothers face legal and emotional challenges:
- Legal Documentation
In the U.S., birth certificates can list intended parents directly, but countries like China require DNA testing for parental recognition. Surrogate mothers must ensure their legal disconnection from the child to avoid custody disputes. - Health Monitoring
Postpartum care should include at least one year of metabolic syndrome screenings. For surrogate mothers carrying multiples, bone density monitoring is critical to address long-term health risks. - Emotional Support
27% of surrogate mothers experience separation anxiety. Agencies now mandate counseling and phased post-delivery communication (e.g., photo updates) to ease emotional transitions.
Section 4: Ethical Controversies Impacting Surrogate Mothers
The surrogacy industry faces four major ethical challenges in 2025:
- Commodification Risks
In Georgia, surrogate mothers receive only 15% of total fees (≈$10,000), while agencies profit margins exceed 300%. Ethical agencies now allocate funds for long-term medical support, such as the “Surrogate Health Fund”. - Eugenics Concerns
While PGT prevents genetic diseases, its misuse for gender selection persists. Ethics committees urge restrictions to medically necessary screenings. - Cultural Exploitation
Surrogate mothers in Middle Eastern programs often face veiling mandates and social restrictions. Contracts must explicitly prohibit such violations of personal freedom. - Legal Loopholes
Cross-border surrogacy leaves surrogate mothers vulnerable in jurisdictions with weak regulations. The proposed 2025 International Convention on Surrogate Rights aims to standardize protections, including age limits (minimum 21 years) and pregnancy caps.
Section 5: Future Trends Shaping Surrogate Mothers’ Roles
Emerging technologies and policies will redefine surrogacy by 2030:
- Artificial Womb Trials
Philadelphia’s 2024 “biobag” experiments with lambs pave the way for human trials by 2030. This technology could reduce health risks for surrogate mothers but raises ethical questions about human dignity. - Blockchain Transparency
Georgia’s pilot program uses smart contracts to automate payments and verify medical records, reducing intermediary exploitation. - Global Ethical Standards
The International Reproductive Ethics Committee (IREC) advocates for the Convention on Surrogate Mothers’ Rights, emphasizing:
- Age and health thresholds for surrogate mothers.
- Mandatory post-surrogacy health tracking.
- Caps on annual surrogate pregnancies.
Conclusion: Balancing Hope and Risk for Surrogate Mother
Surrogacy in 2025 remains a complex interplay of science, law, and ethics. For surrogate mothers, success hinges on:
- Legal Vigilance: Partner with cross-border legal teams to navigate jurisdictional gaps.
- Medical Safety: Choose JCI-accredited clinics and reject underground operations.
- Ethical Advocacy: Demand fair compensation and reject exploitative practices.
Take Action: Visit the International Surrogacy Monitoring Organization (ISMO) for updated agency whitelists and legal guidelines.
Keywords: surrogate mothers, 2025 surrogacy laws, ethical surrogacy, surrogate health, international surrogacy.